 azmy@az-acupuncture.co.uk
|
azmy@az-acupuncture.co.uk
|
 07770 606 674
|
07770 606 674
|
Gaps in knowledge of breast cancer: 
Geriatric Medicine, Volume 43, October 2013.
Ten critical gaps in knowledge about the development of breast cancer must be addressed, including how it evades therapy, according to leading cancer experts.
Projections by Cancer Research UK Show that 185,000 lives will be lost by 2030 at current progress rates in the UK.
A review of evidence by more than 100 scientists, doctors and health care professionals suggests that plugging gaps in research would lead to improved clinical care for patients within 5 years. One of the authors , Prof Alistair Thompson of the University of Dundee said they were beginning to understand some of the greater complexities of what they were dealing with and to unpick some of the mechanisms by which cancer cells work, divide and spread.
The team identified the 10 key gaps that need to be plugged as:
1.Better understanding of genetic factors.
2.Pinpointing sustainable lifestyle changes.
Many studies have shown that overweight and obesity are associated with a modest increase in risk of postmenopausal breast cancer.
The relationship between obesity and breast cancer may be affected by the stage of life in which a woman gains weight and becomes obese. Scientists are actively working to address this question. Weight gain during adult life, most often from about age 18 to between the ages of 50 and 60, has been consistently associated with risk of breast cancer after menopause. (National Cancer Institute at the National Institutes of Health).
Professor Paul Wallace, Drinkaware’s Chief Medical Adviser, believes that more people should know that alcohol can increase women’s risk of getting breast cancer. Although alcohol does increase the risk, taken with all the other factors, its contribution to overall causation of breast cancer is estimated to be only about 4%. The advice is that if you do regularly drink it should be within the government’s daily unit guidelines. The government advises that women should not regularly drink more than the daily unit guidelines of 2-3 units of alcohol (equivalent to a 175 ml glass of wine). ‘Regularly’ means drinking every day or most days of the week (drinkaware.co.uk).
3. Targeted breast screening to those who will most benefit.
4. Understanding how cancer cells grow and spread.
5. Understanding how cancer cells with different characteristics form within a tumour.
6. Tests to measure how well patients respond to chemotherapy or radiotherapy.
7. Improving drug regimens.
8. Developing better imaging techniques.
9. Better practical support.
10. Tissue donation and analysis.
New Guidance on HER (Human Epidermal Growth Factor)2 testing in breast cancer: 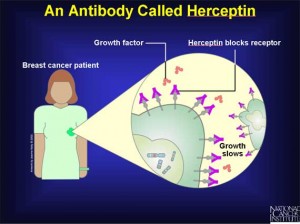
Approximately 15 % of all newly diagnosed breast cancers have HER2-positive, meaning that the tumours are extra copies of the HER2 gene and/or high levels of the HER2 protein, which controls breast cancer cell growth and spread. HER2-positive tumours usually grow faster compared to HER2-negative tumours.
The purpose of HER2 testing is to identify patients who could benefit from effective HER2-trageted therapies such as trastuzumab (Herceptin). These treatments can substantially improve survival in patients with HER2-positive invasive breast cancer. It is therefore important to accurately determine the HER2 status so patients most likely to benefit are offered targeted treatment. At the same time, those that are unlikely to benefit can avoid side effects and costs associated with those drugs.
The American Society of Clinical Oncology (ASCO) and the College of American Pathologists (CAP) recently issued a joint guideline aimed at improving the accuracy and reporting of HER2 testing in patients with invasive breast cancer. They have also developed clinical tools and resources for oncologists and pathologists that summarise the findings and recommendations.
Marlow Complementary Healthcare
c/o Healthy Stuff
Liston Court
Marlow
SL7 1ER
Call : 07770 606 674
Email : azmy@az-acupuncture.co.uk
